Categories
Latest blog
Hydrocolloid dressings are widely used in professional wound care environments, including hospitals, clinics, and home care settings. This article provides an educational overview of when hydrocolloid dressings are commonly used, the types of wounds they are associated with, and key considerations for their appropriate application.
Hydrocolloid dressings are advanced wound dressings made from hydrophilic particles—such as gelatin, pectin, or carboxymethylcellulose—combined with an adhesive backing. When the dressing comes into contact with wound exudate, these particles absorb moisture and form a gel-like layer.
This interaction helps create a moist wound environment, which is widely recognized in modern wound care practices as supportive of the natural healing process. Hydrocolloid dressings are typically occlusive or semi-occlusive, offering protection from external contaminants while allowing limited gas exchange.
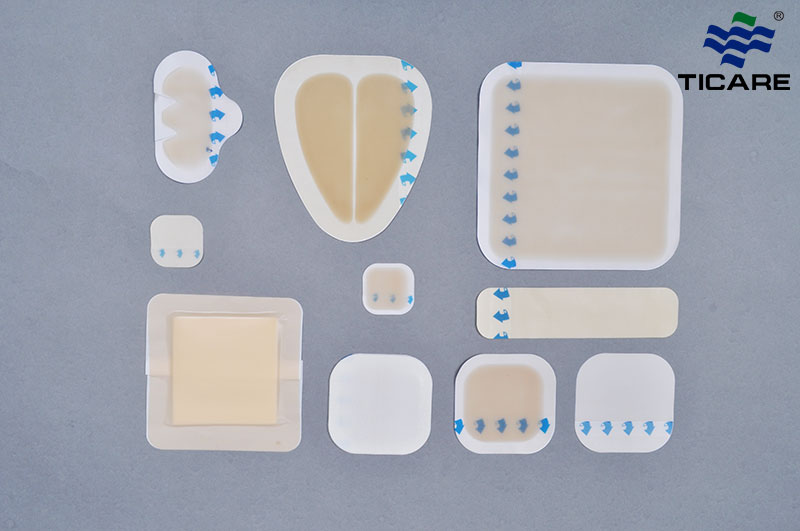
Hydrocolloid dressings are part of a broader range of professional wound care products, each selected based on wound characteristics and care objectives.
In clinical and care environments, hydrocolloid dressings are generally selected based on the following principles:
- The wound requires moisture balance rather than drying
- Protection from friction or external exposure is needed
- Reduced dressing change frequency may be beneficial
- The wound is superficial or partial-thickness
- Professional monitoring of wound progress is available
Hydrocolloid dressings are commonly used as part of an overall wound management plan and are selected according to established wound care practices and professional assessment.
Hydrocolloid dressings are often used for shallow wounds such as minor cuts, abrasions, and superficial skin injuries. Their ability to maintain moisture and protect the wound surface makes them suitable for wounds that do not require heavy exudate management.
In appropriate clinical contexts, hydrocolloid dressings may be used for early-stage pressure injuries, where skin integrity is compromised but deep tissue damage is not present. Ongoing assessment is important to monitor wound progression.
Hydrocolloid dressings are sometimes used to protect closed surgical incisions. In these cases, they help shield the wound from external exposure while maintaining a controlled environment during the early healing phase.
Hydrocolloid dressings are widely associated with blister management, particularly for friction-related skin injuries. The cushioning effect of the dressing may help reduce additional mechanical stress on the affected area.
Hydrocolloid dressings may be considered in situations where:
- Wound exudate levels are low to moderate
- The wound surface is intact or minimally disrupted
- The surrounding skin is in good condition
- A flexible dressing is required to accommodate movement
- The care setting allows for regular wound observation
Selection should always take into account the specific wound condition and care environment.
Before using hydrocolloid dressings, it is important to consider:
- The need for regular wound inspection
- The condition of the surrounding skin
- Signs of increased exudate or wound deterioration
- Compatibility with other wound care materials
- Care protocols in place for dressing removal and replacement
Professional evaluation remains essential when selecting wound dressings, particularly in complex or changing wound conditions.
Hydrocolloid dressings may not be recommended in certain situations, including:
- Heavily exuding wounds
- Deep, tunneling, or cavity wounds
- Wounds showing signs of infection without professional guidance
- Fragile or compromised surrounding skin
- Situations requiring frequent wound visualization
In these cases, alternative wound care products may be more appropriate as part of a comprehensive wound management approach.
Hydrocolloid dressings are one component of a broader wound care system that may include foam dressings, PU films, gauze dressings, and other advanced materials. Effective wound care often involves selecting different dressings as a wound progresses through healing stages.
Medical suppliers typically offer a range of wound care solutions to support diverse clinical and care requirements, enabling healthcare professionals to choose products based on established protocols and patient needs.
Hydrocolloid dressings are widely used in wound care due to their ability to support a moist wound environment and protect the wound surface. Understanding when these dressings are commonly used—and when they may not be suitable—helps support informed and responsible wound care decisions.
For professional applications, hydrocolloid dressings should always be selected based on wound characteristics, care setting, and professional evaluation.
Learn more about our hydrocolloid dressing options designed for professional wound care use.
Hydrocolloid dressings are commonly used in wound care settings where maintaining a moist environment and protecting the wound surface are priorities. They are often selected for wounds with low to moderate exudate and are used under professional guidance as part of standard wound management practices.
Hydrocolloid dressings are typically associated with superficial or partial-thickness wounds, including minor skin injuries and closed wounds. They may also be used in early-stage pressure injuries or friction-related skin damage, depending on wound condition and professional assessment.
In some care settings, hydrocolloid dressings are used to cover closed surgical incisions. Their design allows them to protect the wound from external exposure while maintaining a controlled environment. Selection is based on clinical protocols and the specific characteristics of the surgical site.
Hydrocolloid dressings may be considered for early-stage pressure ulcers where skin damage is limited. Their use depends on factors such as wound depth, exudate level, and monitoring requirements. Ongoing assessment is important to determine whether this dressing type remains appropriate.
Hydrocolloid dressings interact with wound moisture to form a gel-like layer, which helps maintain a moist environment at the wound surface. This environment is widely recognized in wound care practices as supportive of natural healing processes while also providing a protective barrier.
Hydrocolloid dressings may not be suitable for heavily exuding wounds, deep or tunneling wounds, or wounds requiring frequent inspection. They are also generally avoided in situations where infection is suspected without professional guidance, or where surrounding skin is fragile.